The importance of anatomical localization: The Scalenes

When needling, whether it be dry kneeling or acupuncture, precision is key (1, 2). It is often said that "if you don't know where your needle is, you probably shouldn't be there". This is very true and in areas like the apex of the lung field, especially prudent.
The scalene’s are commonly needled muscles, especially for upper extremity radicular pain (3-5), thoracic outlet syndrome (3-7), shoulder pain (3,4,8) , headache, mechanical neck pain (9,10), mechanical dysfunction (10) and altered muscle activation (11,12).
Finding the scalenes can sometimes be challenging. Any methods we can use to improve our precision in needling can only mean better outcomes. I ran across this paper while doing some research for an upcoming lecture (13).
One method is palpating the C1 transverse processes in the area of the mastoid processes and establishing the distance between the lateral tips of the C1 transverse process (C1 TP span) (13) This distance (C1 TP span) should be the same as the distance between the lateral tips of the T1 transverse process (T1 TP span) (13,14). This distance can then be projected to the superior surface of the upper trapezius and one can estimate the T1 TP span and palpate for the position of the first rib lateral to the T1 TP.
A second and potentially easier way is to use the mastoid process (MP) as a landmark. You can use the width of the MP to provide a lateral reference point as you palpate for the first rib through the superior trapezius muscle at a point equivalent to the width of the mastoid processes, approximately 1.3cm lateral to the transverse processes of T1 (15).
Either way will get you there and eliminate a lot of guess work as to where your needle is.
Now that you know where the scalenes are, you can go ahead and needle them. There are several methods to do this.
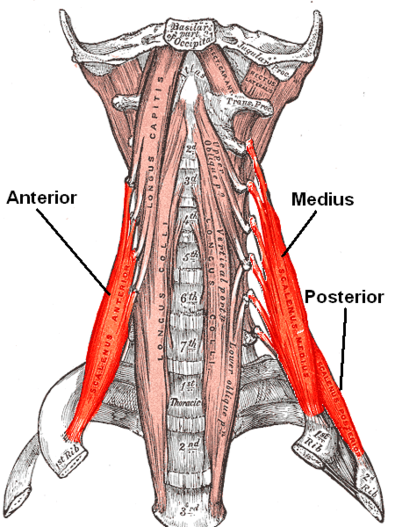
I teach to stay out of the anterior cervical triangle and stay in the posterior occipital triangle, bordered by the posterior border of the SCM, anterior border of the trapezius and superior border of the omohyoid, behind the stereocleidomastoid (16). Use a small needle (15 X 30) and take a perpendicular approach, counting layers and remembering that the anterior scalene lies directly beneath the skin in this area, the middle one layer below it and the posterior, one layer below that. The posterior is rarely needled. The vertebral artery lies within the foramen tranversarium, which lies behind the anterior tubercles where the scalene attach (17). Remember that the anterior scalene attaches from the anterior tubercles of the C3-C6 vertebrae and inserts on the inner border of the 1st rib and the middle, being the largest, attaches from the anterior tubercles of C2-C7 to the upper border of the 1st rib (18). The brachial plexus passes between them. To get to the middle you will have to go through the brachial plexus. This may be an excellent case (ie: middle scalene) for superficial dry needling!
Take home message: this was a lesson in precision and one of the reasons we need to know where our needle is at all times. Use the mastoid to determine the location of the 1st rub and work backward from there.
Keep on needling
Ivo
1. Salvia P, van Sint Jan S, Crouan A, Vanderkerken L, Moiseev F, Sholukha V, et al. Precision of shoulder anatomical landmark calibration by two approaches: a CAST-like protocol and a new anatomical palpatory method. Gait Posture. 2009;29:587–91.
2. Lewit K The needle effect in the relief of myofascial pain. Pain. 1979 Feb;6(1):83-90.
3. Travell JG, Simons DG: Myofascial Pain and Dysfunction: The Trigger Point Manual, Baltimore, Williams and Wilkens, 1983.
4. Flax HJ. Myofascial Pain Syndrome: The Great Mimicker. Bol Assoc Med PR. 1995;87:167–170.
5. Facco E, Ceccherelli F. Myofascial Pain Mimicking Radicular Syndromes. Acta Neurochir. 2005;92(Suppl):147–150.
6. Liebenson CS: Thoracic outlet syndrome: Diagnosis and conservative management. Journal of Manipulative and Physiological Therapeutics, 11(6):493-499, 1988.
7. Roos DB. Thoracic Outlet Syndrome is Underdiagnosed. Muscle Nerve. 1999;22(1):137–138.
8. Fernández-de-las-Peñas C1, Gröbli C, Ortega-Santiago R, Fischer CS, Boesch D, Froidevaux P, Stocker L, Weissmann R, González-Iglesias J Referred pain from myofascial trigger points in head, neck, shoulder, and arm muscles reproduces pain symptoms in blue-collar (manual) and white-collar (office) workers. Clin J Pain. 2012 Jul;28(6):511-8. doi: 10.1097/AJP.0b013e31823984e2.
9. Muñoz-Muñoz S1, Muñoz-García MT, Alburquerque-Sendín F, Arroyo-Morales M, Fernández-de-las-Peñas C. Myofascial trigger points, pain, disability, and sleep quality in individuals with mechanical neck pain. J Manipulative Physiol Ther. 2012 Oct;35(8):608-13. doi: 10.1016/j.jmpt.2012.09.003.
10. Fernández-Pérez AM1, Villaverde-Gutiérrez C, Mora-Sánchez A, Alonso-Blanco C, Sterling M, Fernández-de-Las-Peñas C. Muscle trigger points, pressure pain threshold, and cervical range of motion in patients with high level of disability related to acute whiplash injury.
J Orthop Sports Phys Ther. 2012 Jul;42(7):634-41. doi: 10.2519/jospt.2012.4117. Epub 2012 Jun 7.
11. Florencio LL1, Ferracini GN, Chaves TC, Palacios-Ceña M, Ordás-Bandera C, Speciali JG, Falla D, Grossi DB, Fernández-de-Las-Peñas C Active Trigger Points in the Cervical Musculature Determine Altered Activation of Superficial Neck and Extensor Muscles in Women with Migraine.
Clin J Pain. 2016 Jun 2. [Epub ahead of print]
12. Falla D1, Jull G, Edwards S, Koh K, Rainoldi A. Neuromuscular efficiency of the sternocleidomastoid and anterior scalene muscles in patients with chronic neck pain. Disabil Rehabil. 2004 Jun 17;26(12):712-7.
13. Reichert B. Palpation techniques: surface anatomy for physical therapists. Chapter 11. Stuttgart: Thieme Medical Publishers; 2010. p.288–91.91
14. Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Chapter 26. Upper Saddle River (NJ)Prentice & Hall Health; 2009. p.595
15. Loyd BJ, Gilbert KK, Sizer PS, Atkins LT, Sobczak S, Brismée JM, Pendergrass TJ. The relationship between various anatomical landmarks used for localizing the first rib during surface palpation. J Man Manip Ther. 2014 Aug;22(3):129-33. doi: 10.1179/2042618613Y.0000000064. full text here: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4101551/
16.http://www.med.umich.edu/lrc/coursepages/m1/anatomy2010/html/nervous_system/postneck_ans.html
17. http://www.treccani.it/enciclopedia/nunziante-ippolito_%28Dizionario_Biografico%29/
18. Albertine, David A. Morton, K. Bo Foreman, Kurt H. (2011). "Chapter 25: Overview of the Neck,
