The Tibialis Posterior. Did you know...
Lets take another look at the tibialis posterior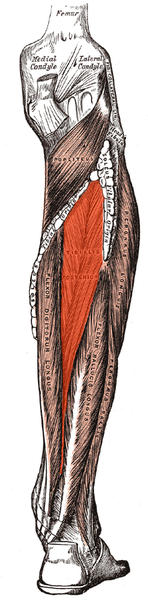 As clinicians , we often needle and treat the tibialis posterior for posterior tibial tendon dysfunction, platar fasicits, patellofemoral joint pain, and a host of other conditions. Lets take a look at some of the anatomy and see why it is a big player in these conditions.
As clinicians , we often needle and treat the tibialis posterior for posterior tibial tendon dysfunction, platar fasicits, patellofemoral joint pain, and a host of other conditions. Lets take a look at some of the anatomy and see why it is a big player in these conditions.
The tibialis posterior takes its origin from the proximal posterior tibia, fibula and inte rosseous membrane. It is deep to the tricep surae and more superior than the flexors hallucis and didgitorum longus. The tendon descends medially, travels around the medial malleolus and divides into 3 portions: plantar, main and recurrent components. It inserts into all the tarsals and metatarsals 2-4.(1) Note that it DOES NOT insert into the 1st. There must be a good reason for this, no?
rosseous membrane. It is deep to the tricep surae and more superior than the flexors hallucis and didgitorum longus. The tendon descends medially, travels around the medial malleolus and divides into 3 portions: plantar, main and recurrent components. It inserts into all the tarsals and metatarsals 2-4.(1) Note that it DOES NOT insert into the 1st. There must be a good reason for this, no?
The tibialis posterior acts to plantar flex and invert the foot as well as help eccentrically control eversion of the foot. It fires from initial conact to almost terminal swing. This assists in plantart flexion of the foot from initial contact to loading response, eccentric slowing of the foot during pronation from loading response to misdstance and concentric contraction to assist in and speed up supination from midstance to terminal stance. When you look at the EMG studies for walking (2,3) , you will see that it starts ramping down activity just after midstance as the peroneus longus starts to ramp up more (firing from just after loading response to pre swing, with a bust of activity from midstance on).
So, with all this talk, there has to be a reason, right? Think about this. In order to move forward in the gravitational plane and have high gear push off (ie, pushing off the base of the hallux), the 1st ray needs to descend to gain purchase on the ground (2,4, 5) . This is largely through the actions of the peroneus longus, extensor hallucis brevis and flexor digitorum brevis (6,7). The function of the peroneus longus should be obvious with its attachment to the base of the 1st metatarsal. The extensor hallucis brevis moves the axis of the 1st MTP downward when it contracts, as discussed here and here (8, 9). The flexor digitorum brevis moves the axis of metatarsal phalangeal joints 2-5 dorsally and posterior which effectively moves the axis of the head of the 1st metatarsal phalangeal joint ventral and anteriorly. This is requisite for you to have adequate hallux dorsiflexion of about 60 degrees to toe off normally.
OK, so what about the tibialis posterior?
Remember that the tib posterior attaches to most of the proximal bottom of the foot with the exception of the 1st metatarsal base? In the area of the 1st ray, the tib posterior attaches to the navicular. When it contracts, it will pull the navicular posterior and inferior, effectively rasing the base of (and lowering the head of) the 1st metatrsal. If it attached to the 1st metatarsal, its base would be pulled posterior and inferior which would raise the head of the 1st ray, exactly what we are trying NOT TO DO.
Armed with this clinical tidbit, can you see how posterior tibial tendon dysfunction can be involved with so many foot and therefore lower kinetic chain problems? If you can’t descend the 1st ray, the foot will need to toe off its lateral aspect, with less effectiveness of the calcaneocuboid locking mechanism (more on that here (10) and here (11)), so problems with propulsion off of an “unlocked” foot. Can you see how the forefoot may be somewhat more everted in this situation? Can you see how this would contribute to more calcaneal eversion and sustained midfoot pronation from midstance through the rest of the gait cycle? What muscle is sitauted to help maintain the arch as well as decelerate pronation? Tibialis posterior. What muscle will be called into play to assist the gastroc/soleus to help propel you forward? Tibialis posterior. You get the picture.
So how do you needle this guy? Start in the mid to upper calf to avoid the sural nerve as it pierces the fascia superficially at the bottom of the calf between the 2 heads. I like to go in laterally and angle the needle medially. Count your layers carefully (more on layers here). You will pierce the fascia, gastroc, soleus and then you are in. If you go deeper and are too medial, you may hit the posterior tibial vessels or tibial portion of the sciatic nerve. If you are trying to avoid multiple insertions, use a longer needle (75mm) and angle inferioly as you work the the muscular dysfunctions.
The tibialis posterior. An important player in the gait game. A great muscle to needle that pays clinical dividends in more ways than you can imagine.
Keep on needling
Dr Ivo
1. Bubra PS, Keighley G, Rateesh S, Carmody D. Posterior Tibial Tendon Dysfunction: An Overlooked Cause of Foot Deformity. Journal of Family Medicine and Primary Care. 2015;4(1):26-29. doi:10.4103/2249-4863.152245.
2. Michaud T. Foot Orthoses and Other Forms of Conservative Foot Care. Thomas Michaud Newton, MA 1993
3. Valmassey R. Clinical Biomechanics of the lower extremities. Mosby, St Louis, Philadelphia. 101-107: 1996
4. Inman VT, Ralston HJ, Todd F. Human Walking. Baltimore, Williams and Wilkins, 1981
5. Scranton PE, et al. Support phase kinematics of the foot. In Bateman JE, Trott AW (eds). The Foot and Ankle. New York, Thieme-Stratton, 1980
6. Perry J. Gait Analysis: Normal and Pathological Function. Thorofare, NJ, Slack 1992
7. The Pathokinesiology Service and the Physical Therapy Department. Observational Gait Analysis. Rancho Los Amigos National Rehabilitation Center Downey, CA 2001
8. https://tmblr.co/ZrRYjxFOn2hk
9. https://tmblr.co/ZrRYjxFSJ4Yz
10. https://tmblr.co/ZrRYjx1MjeIVN
11. https://tmblr.co/ZrRYjxToM8SI
