The Tib Posterior
Posterior tibialis tendinitis is a primary soft tissue tendinopathy of the posterior tibialis that leads to altered foot biomechanics. Although the natural history of posterior tibialis tendon dysfunction is not fully known, it has mostly been agreed that it is a progressive disorder.(1)
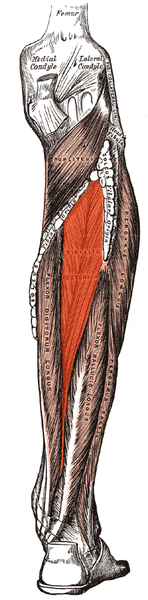 The tibialis posterior originates from the proximal posterior tibia and fibula and interosseous membrane; it is deep in the posterior compartment of the leg and changes its line of pull from the vertical to horizontal at the medial malleolus. The musculotendinous junction is in the distal third of the leg and the tendinous portion turns 90 degrees at the medial malleolus. It has a broad insertion into the plantar surface of the midfoot, largely into the navicular tuberosity with branches to the sustentaculum tali, and the remainder inserting into the entire plantar midfoot except for the 5th metatarsal(1-3).
The tibialis posterior originates from the proximal posterior tibia and fibula and interosseous membrane; it is deep in the posterior compartment of the leg and changes its line of pull from the vertical to horizontal at the medial malleolus. The musculotendinous junction is in the distal third of the leg and the tendinous portion turns 90 degrees at the medial malleolus. It has a broad insertion into the plantar surface of the midfoot, largely into the navicular tuberosity with branches to the sustentaculum tali, and the remainder inserting into the entire plantar midfoot except for the 5th metatarsal(1-3).
The tibialis posterior (TP) is one of the more important extrinsic arch stabilizing muscles. It is a stance phase muscle that fires from the loading response through terminal stance, acts eccentrically to loading response to mid stance to slow pronation and concentrically from mid stance to terminal stance to assist in supination.(4) Its recruitment seems to be increased with slower walking speeds (5).

Since the foot is usually planted when it fires, we must look at its closed chain function (how it functions when the foot/insertion is fixed on the ground), which is predominantly maintenance of the medial longitudinal arch, with minor contributions to the transverse metatarsal and lateral longitudinal arches (6) ; flexion and adduction of the tarsal’s and metatarsals and eccentric slowing of anterior translation of the tibia during ankle rocker. It is also an external rotator of the lower leg and is the prime muscle which decelerates internal rotation of the tibia and pronation. As the origin and insertion are concentrically brought towards each other during early passive heel lift it becomes a powerful plantarflexor and inverter of the rearfoot. There is also a component of ankle stabilization via posterior compression of the tarsal’s and adduction of the tibia and fibula.
Alas, there is much more than the typical open chain functions of plantar flexion, adduction and inversion. Perhaps it is some of these other, closed chain functions, that cause the “progressive nature of posterior tibial tendon dysfunction"(7)?
This muscle is easily accessed through the posterior compartment, lying deep in the midline to the gastroc and soleus (8,9). Care should be taken to avoid the sural nerve, often found between the heads of the gastroc and becoming superficial (and palpable) in the midline where it exits from the inferior junction of the 2 heads of the gastroc (10). The posterior tibial artery, vein and nerve lie on top of the tibialis posterior for the upper 2/3 of its route through the calf, becoming superficial (and palpable) in the distal 1/3 of the lower leg (11). I find starting laterally or medially and angling the needle medially or laterally seems to work best. Make sure to count your layers!
Keep on Needling
Ivo
1. Ling SK, Lui TH. Posterior Tibial Tendon Dysfunction: An Overview. Open Orthop J. 2017 Jul 31;11:714-723. doi: 10.2174/1874325001711010714. eCollection 2017. link to free full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5620404/
10. https://functionalanatomyblog.com/2009/11/26/the-sural-nerve-anatomy-and-entrapment/
11. Enrique Ginzburg, ... Norman M. Rich VASCULAR ANATOMY OF THE EXTREMITIES in Current Therapy of Trauma and Surgical Critical Care, Mosby; Pages 467–472 2008
